Introduction
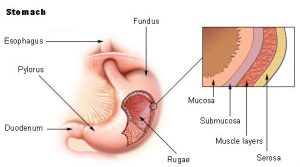
The gastric mucosa secretes 1.2 to 1.5 litres of gastric juice per day. Gastric juice renders food particles soluble, initiates digestion (particularly of protein), and converts gastric contents into a semiliquid mass called chyme, thus preparing it for further digestion in the small intestine. Gastric juice is a variable mixture of water, hydrochloric acid, electrolytes (sodium, potassium, calcium, phosphate, sulfate, and bicarbonate), and organic substances (mucus, pepsin, and protein).
This juice is very acidic due to its hydrochloric acid content and is rich in enzymes. As noted above, the walls of the stomach are protected from digestive juices by the membrane on the surface of the epithelial cells that line the lumen of the stomach; this membrane is rich in lipoproteins, which are resistant to attack by acids. The gastric juice of some mammals (eg, calves) contains the enzyme renin, which binds milk proteins and thus removes them from solution and makes them more susceptible to the action of a proteolytic enzyme.
The gastric secretion process can be divided into three phases (cephalic, gastric, and intestinal) that depend on the primary mechanisms that cause the gastric mucosa to secrete gastric juice. The phases of gastric secretion overlap and there is an interplay and some interdependence between the neural and humoral pathways. The cephalic phase of gastric secretion occurs in response to stimuli received by the senses, that is, taste, smell, sight, and hearing.
This phase of gastric secretion has a completely reflex origin and is mediated by the vagus nerve (tenth cranial nerve). Gastric juice is secreted in response to vagal stimulation, either directly by electrical impulses or indirectly by stimuli received through the senses. Ivan Petrovich Pavlov, the Russian physiologist, originally demonstrated this method of gastric secretion in a now-famous experiment with dogs. The gastric secretion phase is mediated by the vagus nerve and by gastrin release. The acidity of the gastric contents after a meal is buffered by protein, so it generally stays around pH3 (acidic) for about 90 minutes.
Acid continues to be secreted during the gastric phase in response to distension and to peptides and amino acids that are released from proteins as digestion proceeds. The chemical action of free amino acids and peptides stimulates the release of gastrin from the antrum into circulation. Therefore, there are mechanical, chemical, and hormonal factors that contribute to the gastric secretory response to eating. This phase continues until the food has left the stomach.
The intestinal phase is not fully understood due to a complex process of stimulation and inhibition. Amino acids and small peptides that promote gastric acid secretion are infused into the circulation; however, at the same time, the chyme inhibits acid secretion. Gastric acid secretion is an important inhibitor of gastrin release. If the pH of the antral contents falls below 2.5, no gastrin is released. Some of the hormones that are released from the small intestine by the products of digestion (especially fats), notably glucagon and secretin, also suppress acid secretion.
Absorption and emptying
Although the stomach absorbs a few of the products of digestion, it can absorb many other substances, including glucose and other simple sugars, amino acids, and some fat-soluble substances. The pH of gastric contents determines whether some substances are absorbed. At low pH, for example, the environment is acidic and aspirin is absorbed from the stomach almost as quickly as water, but as the pH of the stomach increases and the environment becomes more basic, aspirin is absorbed more slowly.
Water moves freely from the gastric contents through the gastric mucosa into the blood. However, the net absorption of water from the stomach is small because water moves just as easily from the blood through the gastric mucosa into the lumen of the stomach. Absorption of water and alcohol may be delayed if the stomach contains food and especially fat, probably because fat slows gastric emptying and most water in any situation is absorbed in the small intestine.
The rate of emptying of the stomach depends on the physical and chemical composition of the food. Liquids empty faster than solids, carbohydrates faster than proteins, and proteins faster than fats. When the food particles are small enough in size and nearly soluble, and when the receptors in the duodenal bulb (the area where the duodenum meets the stomach) have a fluidity and hydrogen ion concentration of a certain level, the duodenal bulb and the second part of the duodenum relax, allowing emptying of the stomach to begin.
During a duodenal contraction, the pressure in the duodenal bulb increases more than in the antrum. The pylorus prevents reflux into the stomach by closing. The vagus nerve plays an important role in voiding control, but there are indications that the sympathetic division of the autonomic nervous system is also involved. Several of the peptide hormones of the digestive tract also have an effect on intragastric pressure and gastric movements, but their role in physiological circumstances is unclear.
